Stem cells are the cells responsible for producing new cells. This is important for growth, replacement, and repair. Here, we give you a short overview of different stem cell types before comparing the progress made towards therapies for patients, and the challenges or limitations that still need to be addressed.
What are stem cells?
Stem cells are the body’s natural reservoir for cell growth and repair. They replace specialised cells that have been lost to use or damage
We need to make new cells all the time, just to keep our body functioning. Some specialised cells (such as blood and muscle cells) are unable to make new copies of themselves through cell division. Instead, they must be replenished from populations of stem cells.
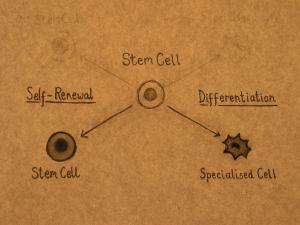
Stem cells have the unique ability to produce both copies of themselves (self-renewal) and other more specialised cell types (differentiation) when they divide. Which path they follow depends on the need of the body.
Stem cells are essential to the maintenance of tissues such as blood, skin, and gut that undergo continuous turnover (cell replacement), and muscle, which can be built up according to the body's needs and is often damaged during physical exertion.
What makes stem cells unique?
Stem cells are unspecialised. Unlike a red blood cell, which carries oxygen through the blood stream, or a muscle cell that works with other cells to produce movement, a stem cell does not have any specialised physiological properties. These cells are said to be undifferentiated.
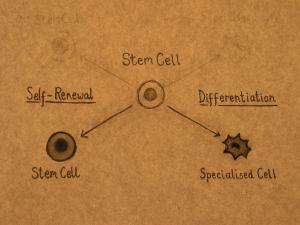
Stem cells can divide and produce identical copies of themselves over and over again. This process is called self-renewal and continues throughout the entire life of the organism. Self-renewal is the second of the three defining properties of stem cells. Specialised cells such as blood and muscle do not normally replicate by producing copies of themselves. This means that when they are seriously damaged by disease or injury, they cannot replace themselves.
The third defining property of stem cells is the ability to produce more specialised cell types within the body. This process is called differentiation or maturation. Stem cells in different tissues vary in the number and types of cells that they can produce. For example, male germline stem cells make only sperm, but they are stem cells: they are undifferentiated, can self-renew, and make the specialised cells, sperm.
What are the different types of stem cells?
Many people think that stem cells come from an early embryo, and that they can be turned into any type of cell. This is not true of all stem cells. In fact, we have stem cells in our bodies all our lives.
Stem cells can be divided into three categories:
1. Embryonic stem cells These are cells which have been grown in the laboratory, after being taken from the early embryo. These can turn into any type of specialised cell.
2. Induced pluripotent stem cells: These are former specialised cells, collected from an adult, which were ‘de-differentiated’ in the laboratory to return them to an undifferentiated or unspecialised state. They are similar to embryonic stem cells in that they can turn into any type of specialised cell. The laboratory technique used to make these cells was discovered in 2006. These are also known as iPS cells, iPSCs, or ‘reprogrammed’ stem cells.
3. Tissue-specific stem cells: These are cells found in our bodies throughout our lives. They are not able to make any type of cell, but they are often able to make multiple cells types to replenish the tissue they are associated with. These are also known as ‘adult stem cells’.
You can read in more about the properties of these different types of stem cells and current research work in our other factsheets.
Embryonic stem cells (ESCs)
Pluripotent stem cells can make any type of specialised cell in the body (eg., embryonic stem cells). Multipotent stem cells can make several different specialised cells (eg., haematopietic stem cells). Unipotent stem cells are responsible for producing a single type of specialised cells (eg., germline stem cells).
Embryonic stem cells (ESCs) have unlimited potential to produce specialised cells of the body. This suggests enormous possibilities for disease research and for providing new therapies. ESCs are pluripotent: they can differentiate into any cell type of the body.
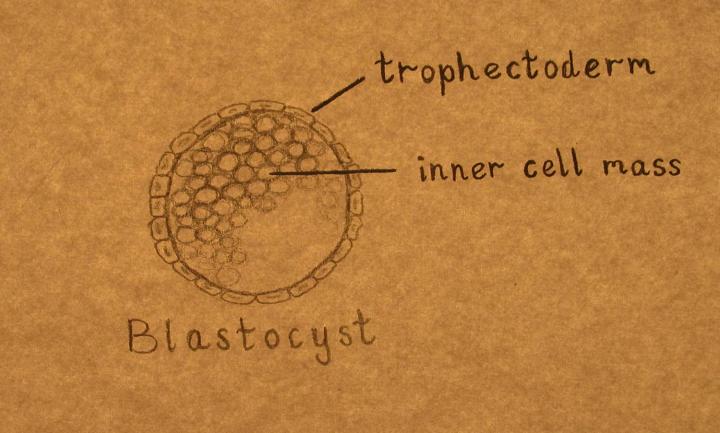
Human ESCs were first grown in the lab in 1998. These cells are derived from a very early stage of development. The embryo consists of about 100 cells, forming a structure called a blastocyst, and has not yet implanted into the uterus.
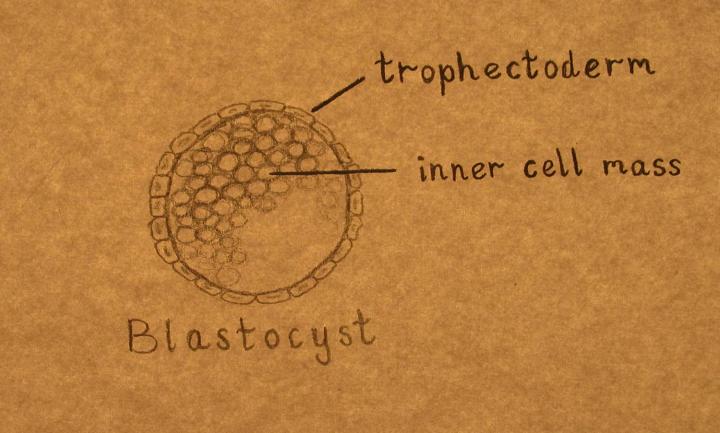
Not every experiment using ESCs requires a new blastocyst. ESCs derived in the lab can be maintained and grown in large numbers for long periods of time. In fact, it seems possible to continue growing them indefinitely. When scientists know that a particular group of ESCs can be maintained and grown indefinitely, they can save samples to deposit in stem cell banks, so that other scientists can use them too. These saved samples are referred to as cell lines. Cell lines are often used in the early stages of experiments, as their properties are well-known, and it makes it easier to compare results between other trials using the same line.
ESCs can be used to study how specific tissues develop. They can also be used for drug-testing, and for modelling diseases in different tissues without collecting tissue samples from patients.
There are still some practical challenges around the use of ESCs for research or in the clinic. Researchers need to ensure that ESCs fully differentiate into the required tissue type, and that tissues grown from ESCs will behave the same way as those which grow in the body. There are also ethical considerations around the use of cells obtained from a human blastocyst.
Induced Pluripotent Stem Cells (iPSCs)
In 2012, Shinya Yamanaka and John B. Gurdon received the Nobel Prize for their discovery of iPSCs.
The discovery that specialised, mature adult cells can be ‘reprogrammed’ into cells that behave like embryonic stem cells was a breakthrough in the field of stem cell research. This process is sometimes called de-differentiation.
iPSCs offer a source of ESC-like cells which can be accessed without the creation of a blastocyst. They can used to study developmental process, the factors involved in the growth of specific tissue types, and as a way of modelling diseases in the lab.
From the clinical perspective, the discovery of these induced pluripotent stem cells (iPSCs) raised hopes that cells could theoretically be made from a patient’s own skin (or other tissues) in order to treat their disease. This would avoid the risk of immune rejection. It may also the generation of iPSC cell banks, which would function like blood banks: matching patients with suitable donors.
Similar to ESCs, iPSCs must be shown to completely and consistently differentiate into the required types of specialised cells to make them effective tools for research, and eventually to meet standards suitable for use in patients.
Tissue-specific (adults) stem cells
Many tissues in the human body are maintained and repaired throughout life by stem cells. These tissue-specific stem cells are very different from embryonic stem cells.
Tissue-specific stem cells are not pluripotent like ESCS. They have partially differentiated or matured, and so they are no longer capable of producing everyu cell type. They are still capable of self-renewal. Most adults stem cells are multipotent, capable of producing only a limited number of specialised cell types. Some are even unipotent: they produce only one type of cell.
Adult stem cells can only make a limited number of specialised cell types. For example, neural stem cells can only differentiate into brain cells; haematopoietic stem cells (blood stem cells) can only differentiate into specialised blood and immune cells; and germline cells can only produce sperm or ova.
How do all these types of stem cells compare?
Stem cells are important tools for disease research and offer great potential for use in the clinic.
Currently, the major use of ESCs and iPSCs is in disease modelling, drug testing or to increase our understanding of the basic biology of this cell type.
Some adult stem cell sources are currently used for clinical purposes, such as haematopoietic blood stem cell transplant (also called a blood stem cell transplant, or bone marrow transplant.)
As of 2023, 100 cases of clinical studies using ESCs/iPSCs have been carried out or are ongoing. Much more time study is needed before any therapeutics for more patients can be approved.