Over 400,000 people in Europe have multiple sclerosis (MS). It can cause blurred vision, extreme fatigue, pain, numbness, loss of movement, and balance problems. There are generally three main disease courses: relapsing-remitting MS, secondary progressive MS and primary progressive MS. MS is the most common disease-causing disability in young adults. There is currently no cure. Scientists are investigating whether stem cell and gene therapy techniques can be used to support people living with MS.
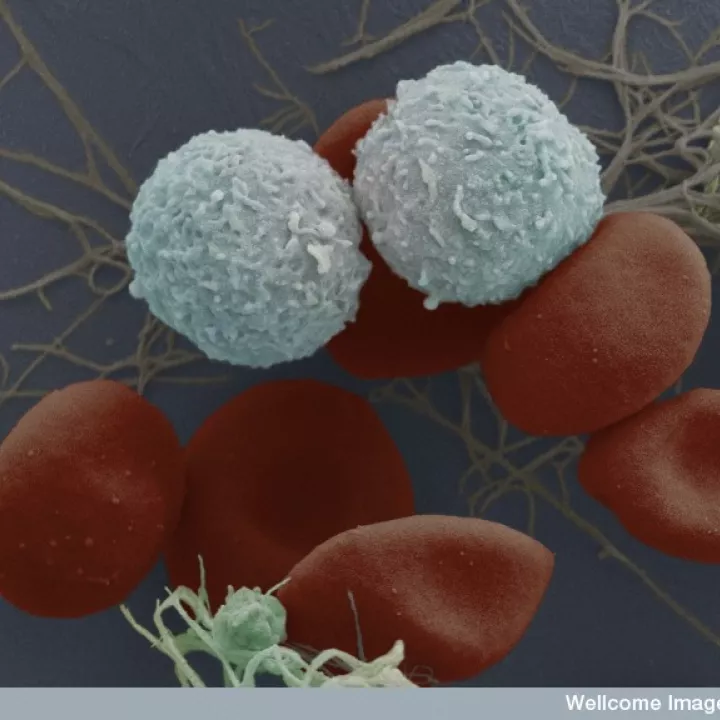
Blood stem cells are found in the bone marrow. They differentiate in different types of immune cells, involved in causing the damage in MS.
MS patients have been given transplants of their own blood stem cells in an attempt to ‘reset’ the immune system. Blood stem cells are collected from the patient’s bone marrow. The patient’s existing immune cells are then killed using chemotherapy (treatment with powerful medicine). The patient’s blood stem cells are then injected into the blood stream, with the aim of generating new immune cells that will not attack the myelin. This method has been shown highly effective in relapsing-remitting MS patients, but not in progressive MS patients. The treatment has improved with safety over time, with ongoing improvements in treatment-related mortality rates (from 7.3% of the earliest use of the treatment during 1995–2000; 1.3% during 2001–2007; 0.7% during 2008–2016; and down to 0.2% after 2016. Data from EBMT Registry). However, it is still a risky procedure; as it involves the suppression of the immune system, it makes infections likely. It is therefore being used for patients with highly active forms of multiple sclerosis which do not respond to the best available drug therapies.