Reprogramming allows us to turn any cell of the body into a pluripotent stem cell, and then into any other type of cell. The discovery of reprogramming in 2006 changed the scientific community’s thinking about how cells work. Reprogramming has opened up exciting possibilities for studying and treating disease.
What do we know?
Pluripotent stem cells are cells which have the potential to turn into any cell in the body.Embryonic stem cells (ESCs) were thought to be the only source of pluripotent cells. However, in 2006, Kazutoshi Takahashi and Shinya Yamanaka showed that skin cells can be reprogrammed into ‘induced’ pluripotent stem cells (iPSCs) by artificially adding four genes.
Researchers have been excited by the opportunities iPSCs offer for studying, treating and potentially curing diseases. Because iPSCs come from adult cells, they avoid several moral issues that accompany the use of ESCs.
iPSCs offer researchers an excellent way to create and study diseased cells that contain the same genes as individual patients.
What are researchers working on?
Researchers are constantly working to better understand how cell reprogramming works in order to develop better methods for controlling stem cell differentiation.
iPSCs are being used to study and develop treatments for many diseases. Scientists are studying whether they can be used to replace cells destroyed by diseases.
The genetic errors which cause specific diseases often vary from patient to patient. IPSCs could be used to develop bespoke treatments to fix a patient’s specific genetic problems. An added benefit is that transplantations of iPSCs will not be rejected by a patient’s immune system, because iPSCs are created from a patient’s own cells.
What are the challemges?
Several studies show that iPSCs and ESCs often function differently. This is probably because iPSCs are not truly ‘100%’ reprogrammed. Researchers are still determining the effect of these differences on research and medicine.
Technical challenges and our limited understanding of iPSCs make it difficult to control stem cells, and how cells made from iPSCs will behave in the body.
Although medical treatments using customised iPSCs may sound attractive, developing affordable and effective iPSC treatments remains a very large challenge.
Discovery of iPS cells
In 2006, Shinya Yamanaka made a ground-breaking discovery. He found a new way to ‘reprogramme’ adult, specialised cells and turn them back into stem cells. These laboratory-grown stem cells are pluripotent – they can make any type of cell in the body - and are called induced pluripotent stem cells, or iPS cells. Only embryonic stem cells (ESCs) are naturally pluripotent. Yamanaka’s discovery means that, theoretically, any dividing cell of the body can now be turned into a pluripotent stem cell. He was awarded the Nobel Prize in Physiology or Medicine just six years after this discovery.
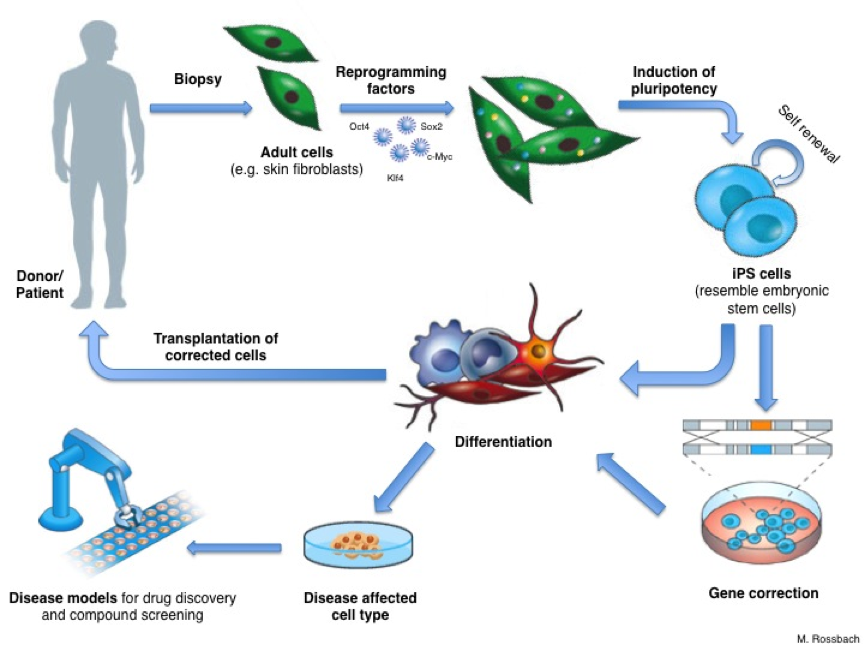
So how are iPS cells made? Yamanaka collected mouse skin cells, added four genes, and grew these altered cells in the laboratory. This started a process inside the cells called reprogramming or dedifferentiation. Within 2 – 3 weeks, the skin cells were converted into induced pluripotent stem cells. Scientists can now also do this with human cells, by adding even fewer than four genes.
iPS cells and disease

Shinya Yamanaka first discovered iPS cells in 2006 and won a Nobel Prize for the work in 2012
An important step in developing a therapy for a given disease is understanding exactly how the disease works. What exactly goes wrong in the body, and where? To do this, researchers need to study the cells or tissues affected by the disease. This is not always as simple as it sounds.
For example, it’s almost impossible to collect brain cells from patients with Parkinson’s disease, especially in the early stages of the disease before the patient is aware of any symptoms. Reprogramming means that scientists can now get access to large numbers of the type of neurons (brain cells) that are affected by Parkinson’s disease. Researchers first make iPS cells from, for example, skin biopsies (of specialised cells) from Parkinson’s patients. They then use these iPS cells to grow neurons in the laboratory. The neurons have the same genetic make-up as the patients’ own cells. This way, scientists can directly work with neurons affected by Parkinson’s disease in a dish. They can use these cells to learn more about what goes wrong inside the cells and why. Cellular ‘disease models’ like these can also be used to search for and test new drugs to treat or protect patients against the disease.
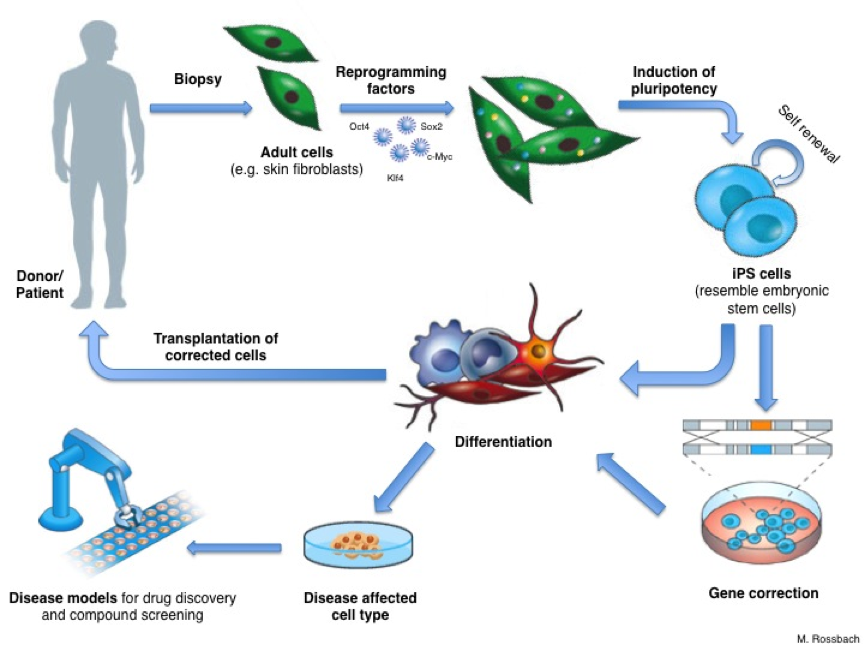
iPS cells - derivation and applications: Certain genes can be introduced into adult cells to reprogramme them. The resulting induced pluripotent stem cells resemble embryonic stem cells and can be differentiated into any type of cell to study disease, test drugs or-after gene correction-develop future cell therapies
Future applications and challenges
Reprogramming holds great potential for new medical applications, such as cell replacement therapies. Since iPS cells can be made from a patient’s own skin, they could be used to grow specialised cells that exactly match the patient. This means they would not be rejected by the immune system.If a patient has a genetic disease, the genetic error could be corrected in their iPS cells in the laboratory. These ‘corrected’ iPS cells could be used to grow a patient-specific batch of healthy specialised cells for transplantation. But this benefit remains theoretical for now.
Until recently, making iPS cells involved permanent genetic changes inside the cell. These changes can cause tumours to form. Scientists have now developed methods for making iPS cells without this genetic modification. These new techniques are an important step towards making iPS-derived specialised cells that would be safe for use in patients.
Further research is now needed to understand fully how reprogramming works and how iPS cells can be controlled. This will allow researchers to develop cells which are consistent in their behaviour. This is essential to meet the high quality and safety requirements for use in the clinic.