Embryonic stem cells have captured the imagination of scientists and non-scientists alike. But what are they, where do they come from and why are researchers all over the world working hard to understand more about them?
What do we know?
Human embryonic stem cells (ESCs) are pluripotent cells. This means that they can that can make any type of cell in the body. They are made from cells found in very early human embryos, before they have implanted in the uterus. At this pre-implantation stage, the embryo is called a blastocyst.
Many areas of science use mouse ESCs to study how mammalian embryos develop. They are also used to investigate what signals direct stem cells to differentiate into specialised cells.
ESCs have been used to study healthy development, and the development of diseases. Scientists can use gene editing techniques to create genetically modified mice. Researchers can then study these mice to understand how specific genes contribute to different cell functions, and to diseases. An extremely useful research tool is the use of chimaeras. These are animals which have had their own ESCs ‘'mixed’ with ESCs modified in the lab, so that both types help to build the body.
What are researchers working on?
Researchers are learning how to create many different specialised cell types found in the body. They do this by exposing ESCs to different chemical signals and growth conditions. Many tissues, such as nerves and muscles, can now be grown from ESCs in a lab outside the body.
Mouse ESCs are being used to learn about how the body develops, from early embryonic stages to the formation of complex organs. Scientists can study early developmental process outside the body by growing them in suspension (floating in a liquid containing nutrients). ESCs grown this way aggregate (form clumps of cells). Scientists can use these cell aggregates to recreate and investigate early developmental processes.
These ESC aggregates can even undergo gastrulation. This is the process in which the cells start turning into different ‘types’ of tissue: ectoderm (neurons and skin), mesoderm (heart and muscle), and endoderm (gut). Researchers are learning how cells assemble into complex tissues, such as the layers of the brain, by attempting to grow primitive organs in the lab. Specific tissues grown from ESCs in the lab can be used to screen drugs for toxicity or other effects.
Many studies are looking into how ESCs might be able to be used to treat numerous different diseases, from multiple sclerosis to blindness and diabetes.
What are the challenges?
There are differences between how ESCs function for mice and humans. For moral and ethical reasons, researchers cannot use human ESCs as they do in experiments with mouse ESCs. This is especially true in the context of chimaeras. This requires researchers to figure out how human ESCs work in more complex and indirect ways.
Another challenging area is controlling exactly how ESCs differentiate into numerous specialised cell types.
Finding ways to get large yields of specialised cells made from stem cells that are uniform and give reliable results is a major goal, but not one that is easy to achieve. This is because during development, the formation of most specific tissues depends upon signals coming from a neighbouring tissue or organ.
The origin of embryonic stem cells
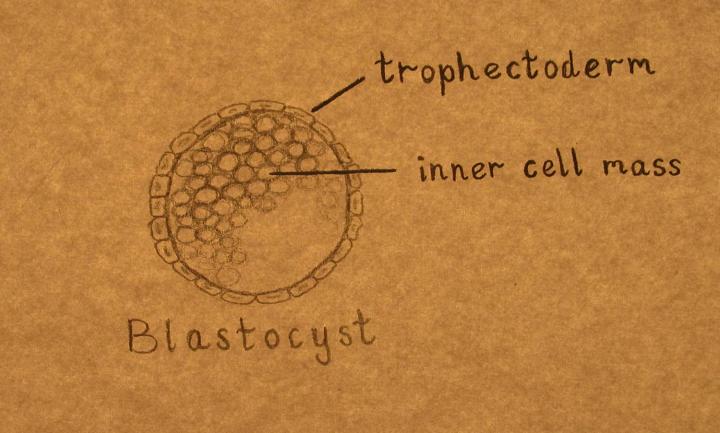
Embryonic stem cells are grown from cells found in the embryo when it is just a few days old, before it has implanted into the uterus. In humans, mice and other mammals, the embryo is a ball of approximately 100 cells at this stage. It is known as a blastocyst and has two parts: the inner cell mass and the trophectoderm.
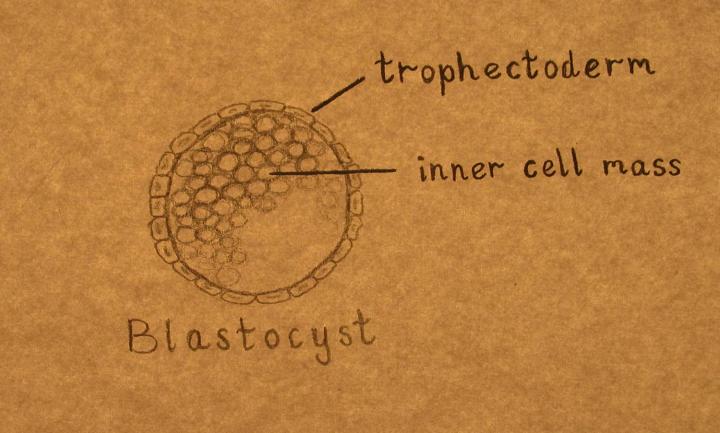
The outer layer of cells (trophectoderm) will form the placenta, which supports the embryo as it grows inside the uterus.
The inner clump of cells (the inner cell mass) is a ball of 10–20 cells. These cells are undifferentiated, or unspecialised. They will multiply and differentiate extensively to make the many types of cells needed to form the entire body. Some of the cells in the inner cell mass are pluripotent. This means they can make every type of cell in the body.
Mouse stem cell basics
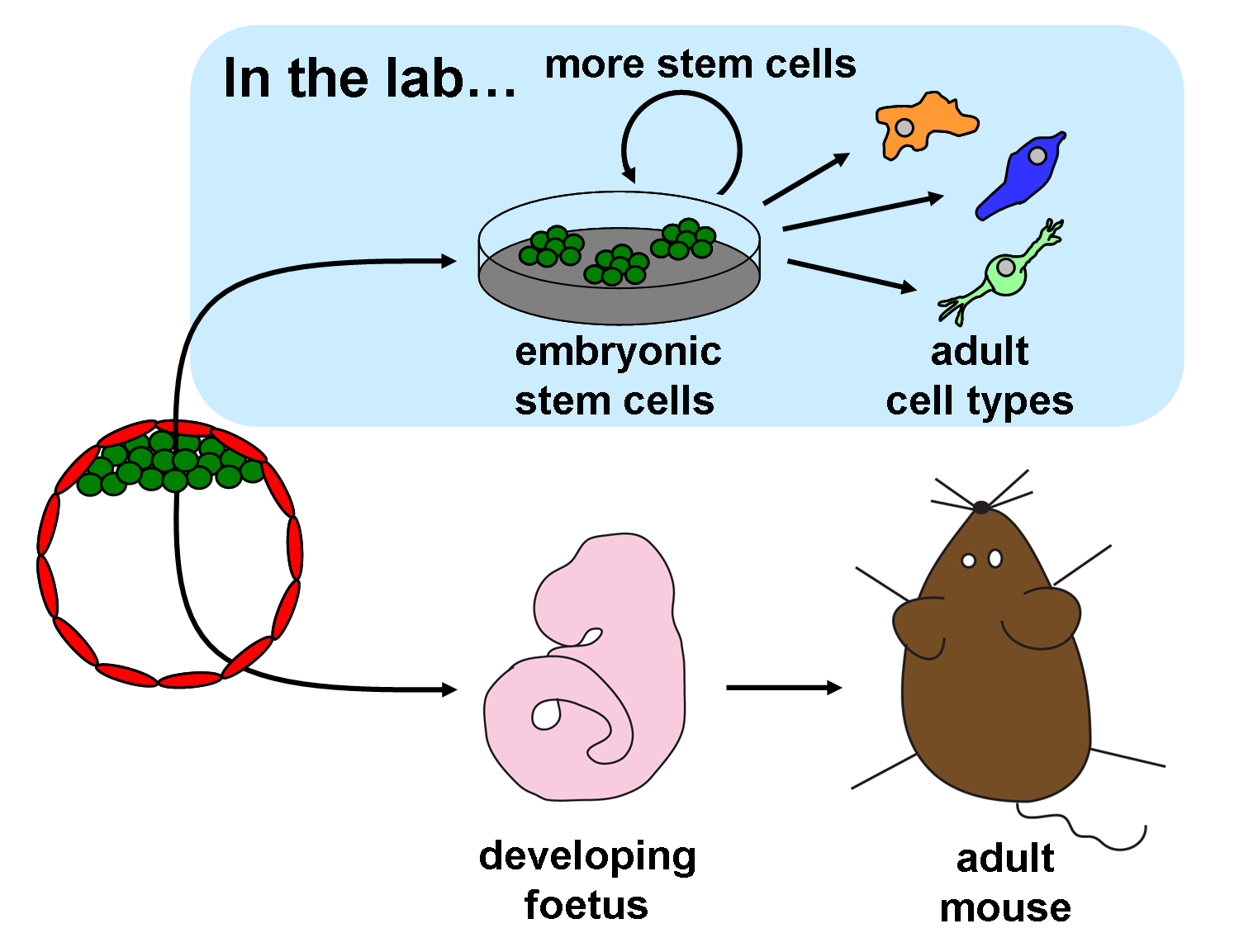
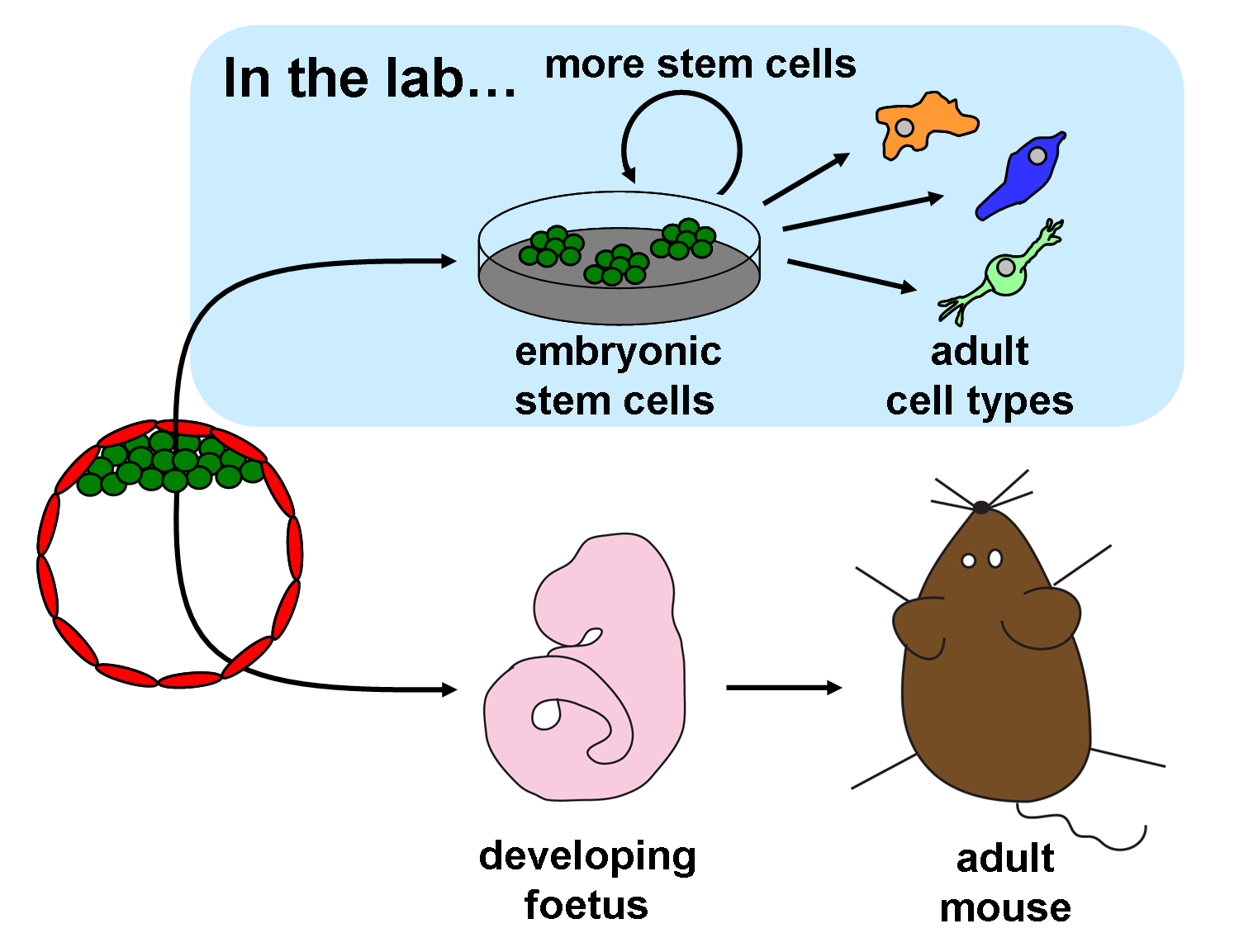
If an inner cell mass is taken from a mouse blastocyst and given the right nutrients and signals to prevent differentiation, the pluripotent cells can grow in the laboratory. The process of cell maturation and specialisation that would normally take place in the embryo stops. Instead, the cells multiply to make greater numbers of undifferentiated cells that resemble the cells of the inner cell mass. These laboratory-grown cells are called embryonic stem cells (ESCs).
Using mouse embryonic stem cells for science and medicine
Mouse ESCs grown in the lab can be injected back into a mouse blastocyst, and this blastocyst can then be returned to the uterus of a female mouse to develop into a foetus. The injected ESCs take part in the development of the foetus and the resulting pup is born with a mixture of cells: those from the host blastocyst and those that came from the injected ESCs. This new mouse with cells from two different origins is known as a chimaera.
Researchers can precisely alter the genes of ESCs cells in the lab, put the cells back into blastocysts, and produce new chimaera mice that contain the modified genes. These chimaera mice can pass genes from ESCs on to their offspring, producing some mice which have only the altered gene.
Scientists use genetically altered mice made from ESCs to study genes involved in many human diseases. For example, they have made mice with mutations found in human cancers. These mice can be studied to learn more about how cancers grow and to test potential drugs. The immense value of this technique for science and medicine was recognized in 2007 when the Nobel Prize in Medicine was awarded to three scientists who pioneered the use of ES cell to create genetically modified mice.
Human embryonic stem cells
Scientists have also made ESCs from the inner cell masses of human embryos by employing a similar technique to that used to isolate mouse ESCs.
It is not not legal to inject human ESCs back into blastocysts. However, these cells can be differentiated in the laboratory to make many different specialized cell types. By using human ESCs to produce specialized cells like nerve cells or heart cells in the lab, scientists can access adult human cells to study without taking tissue from patients. They can then study these specialized adult cells in detail to see what goes wrong in certain diseases, or to study how the cells respond to potential new drugs. Scientists are also starting to develop therapies for certain diseases (e.g. age-related macular degeneration and Parkinson’s) using cells derived from ESCs.
What's next?
Human and mouse ESCs have some different properties. Scientists are trying to understand why this is and whether human cells can be obtained with the same properties as the mouse ESCs.
Researchers are also working to expand and perfect methods for making specific adult cell types from ESCs in the lab. Controlling exactly how ESCs differentiate is still a major challenge. Even so, some scientists are already investigating whether ES cells can be used to make adult cells that could be transplanted into patients to help heal injured or diseased tissue.